The Big Picture
Hospitals today are facing greater pressure to deliver high-value services, in conjunction with excellent patient care experiences. Yet, decreasing revenues, increasing costs, and growing expectations from patients create a challenging environment. Hospital executives are investigating alternative approaches that drive continuous improvement in an environment that is changing more rapidly than ever.
A recent study by The Advisory Board showed that hospital CFOs view reduction in care variation as their single most important cost improvement opportunity. How much are the savings?
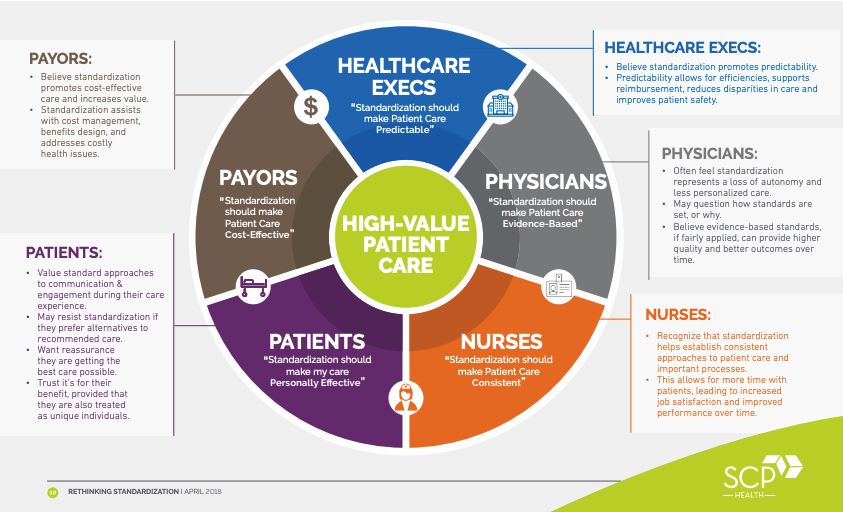
Despite the opportunity, truly successful and sustainable strategies that improve standardization of care are still elusive to health systems and their leadership teams. A primary reason most approaches have failed is that the unique contributions and perceptions of key stakeholder groups were not acknowledged or well-balanced.
Successfully creating material improvements in value through standardization means leveraging the skills, experience, data, and leadership from all members of the care team, including the key stakeholders who impact patient care.
In this whitepaper you’ll find:
- The most common challenges to standardization initiatives
- A new framework for engaging five stakeholders
- Recommendations for an effective approach to leveraging data and feedback systems
- The key role of clinical partnership in the quest for effective standardization
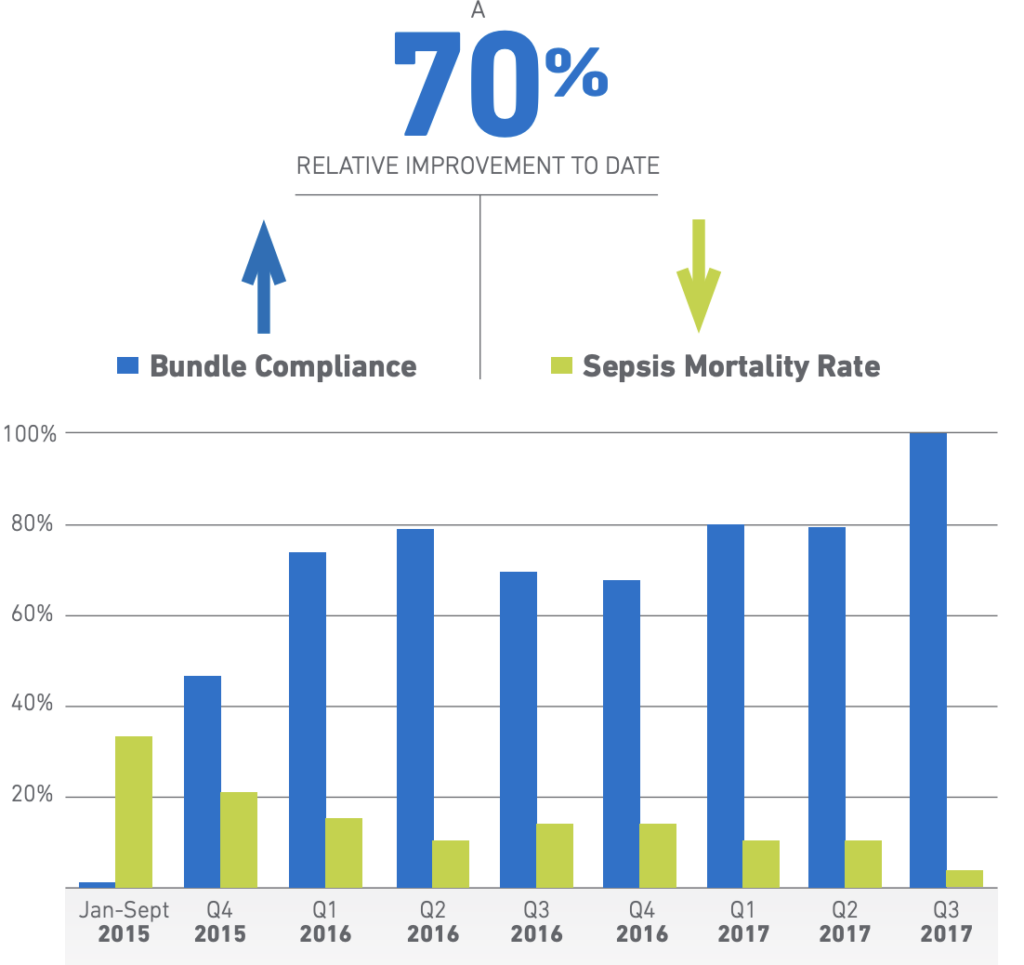
- Examples of success in two of the most critical elements of hospital-based care: Emergency Departments and Hospital Medicine programs