Introduction
It was just over twenty years ago when the Hospital Medicine specialty began to emerge. Since 2003, the number of hospitalists has grown by more than five times. Though its growth has been enormous and its practitioners are highly respected, Hospital Medicine (HM) is a very young specialty and most programs have significant opportunities to further evolve. This reality was made clear with the COVID-19 pandemic, as many healthcare organizations rushed to set up a structure that could handle such a large-scale global crisis. Though we can never fully prepare for something of this magnitude, there are several steps hospital leaders can take to build a well-equipped program ready to navigate these types of unforeseen challenges. The first is to develop a tailored strategy to capitalize on the potential of Hospital Medicine and expand its impact. In this white paper, readers will gain a deeper understanding of:
- the beginnings of HM and how that colors the way the specialty is practiced today,
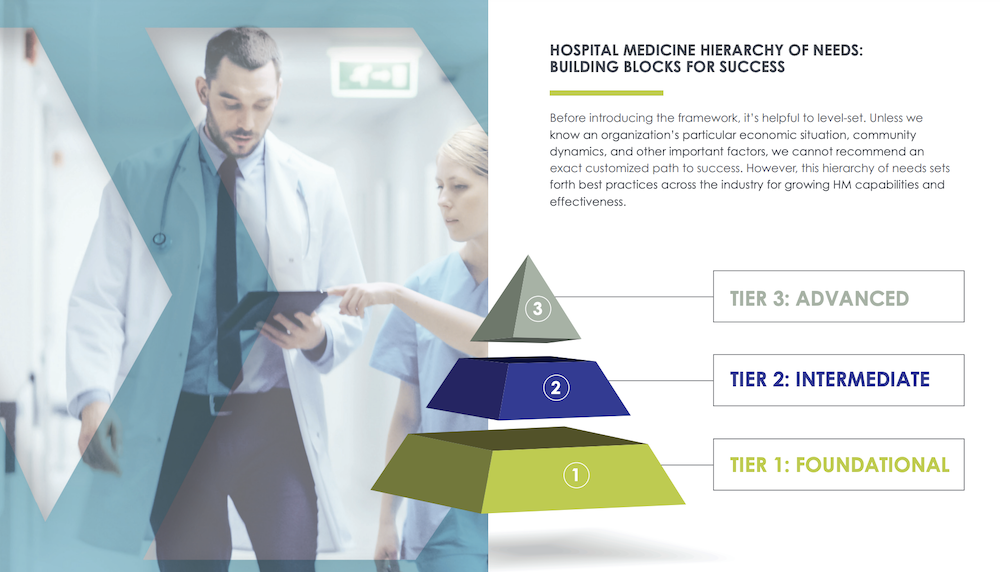
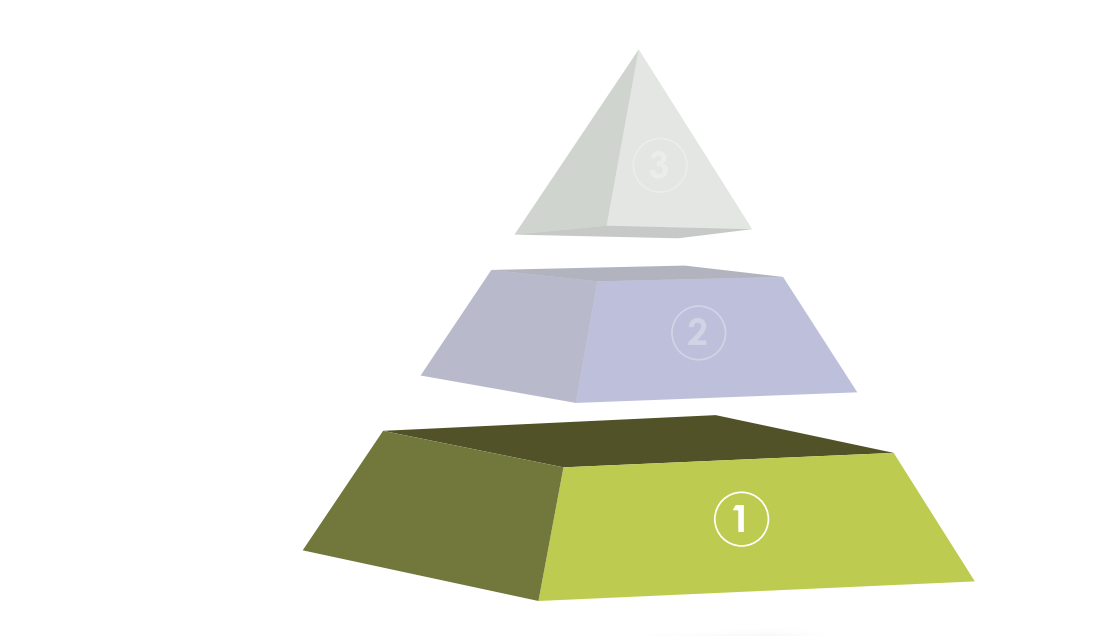
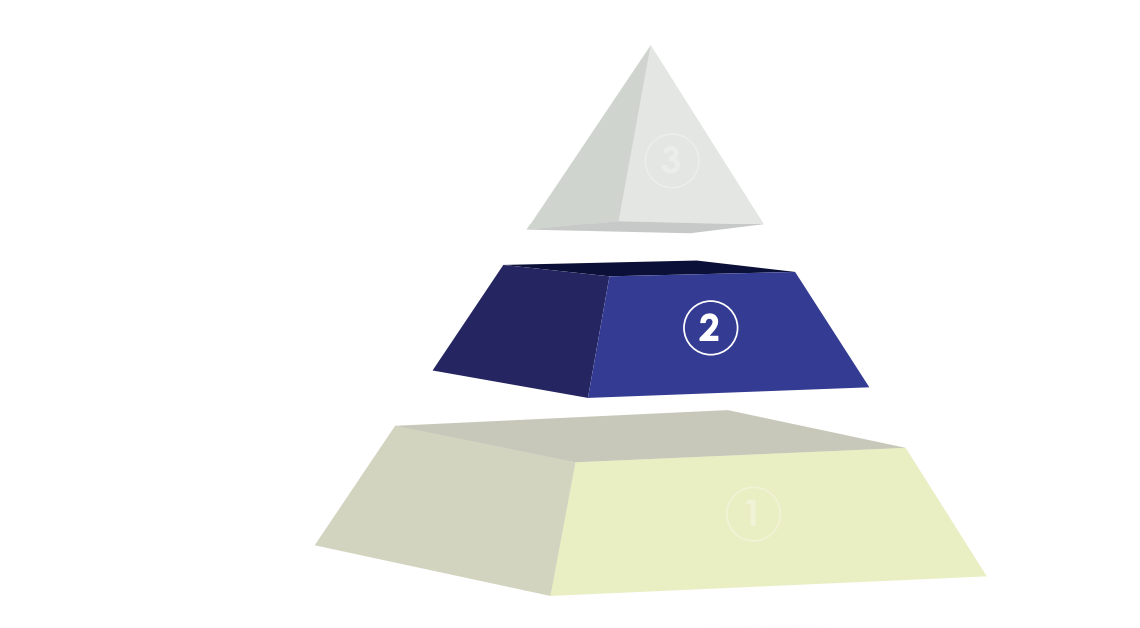
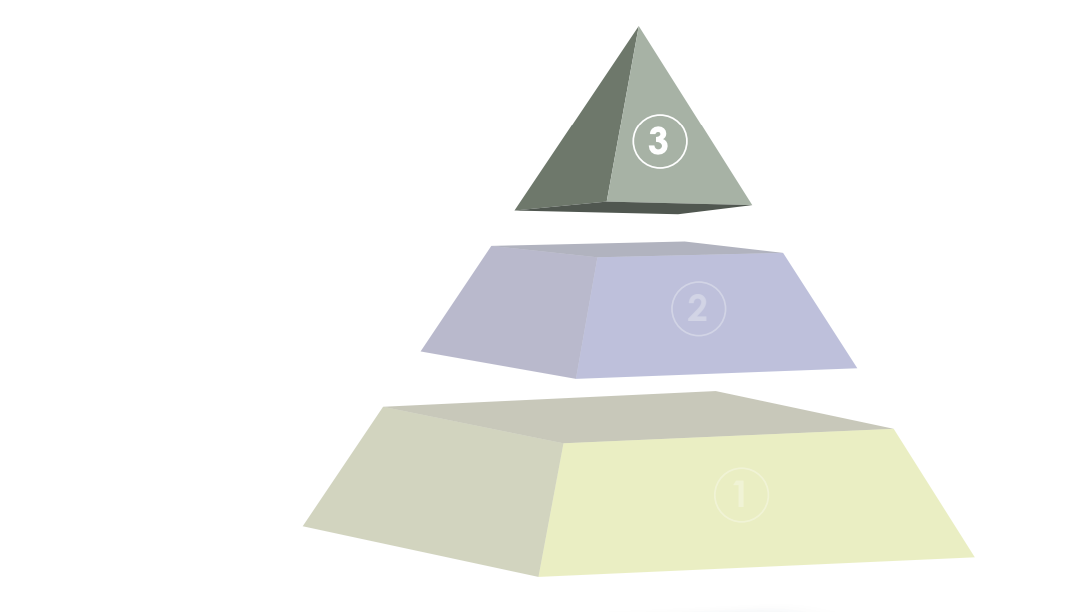
- our tiered model of HM program development— and how to evaluate where a program lands,
- how other hospitals are approaching HM advancement, and
- what is needed to navigate the future of inpatient care.
Ultimately, this white paper provides an opportunity to gain a better grasp on the evolution of HM, what success looks like in the current landscape, and how HM programs and hospitalists can prepare for the next generation of the specialty.