An actionable JOC plan, including meeting agenda items, a joint standards checklist, and examples from the field.
Formalizing Shared Goals + Achieving Performance Improvements
Hospitals charge emergency medicine physicians and hospitalists with the same goal: to provide the best care possible for their patients at all times. However, these two groups can find themselves working in opposition to one another due to conflicting priorities.
Compromised cost efficiency, patient experience, patient safety, physician satisfaction, and care consistency are all consequences of EM and HM programs that find themselves at loggerheads with one another. Conversely, when the two programs are aligned, care quality and efficiency improve.
In our first guide to EM & HM collaboration we introduced the concept of a Joint Operations Committee or JOC – a proven, effective way to bring the two programs together and maintain cohesion. In this companion guide, you’ll find detailed strategies for setting up a JOC, expectations for performance improvements, and examples from the field from a hospital program case study.
In this companion guide, you’ll find detailed strategies for setting up a JOC, expectations for performance improvements, and examples from the field from a hospital program case study.


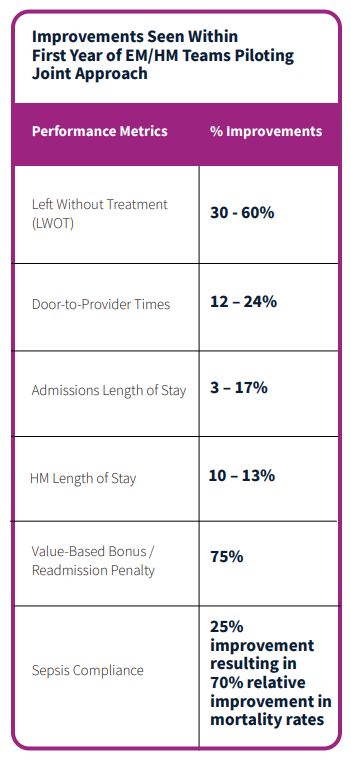 Facilities that institute a new process to formalize a JOC and make a concerted effort to align their EM/HM programs typically see performance improvements within 90-120 days. Example improvements seen within the first year (from actual experience using established methods) include
Facilities that institute a new process to formalize a JOC and make a concerted effort to align their EM/HM programs typically see performance improvements within 90-120 days. Example improvements seen within the first year (from actual experience using established methods) include



