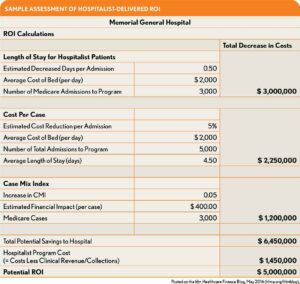
As Medicare payment dependency on performance metrics increases, hospital administrators are being forced to take a microscopic look at the costs of supporting clinical service lines regarding both patient care and ROI.
As a hospitalist, you manage a large percentage of all medical and surgical patients and, therefore, play a key role in determining whether the hospital will avoid penalties or, in the case of value-based purchasing, earn bonus dollars.
In this post, we discuss six HM program economic and behavioral value drivers you can put into action to improve patient outcomes and significantly impact ROI.
Value Driver #1: Optimize EM-HM Transitions of Care
Emergency and Hospital Medicine programs function best when they work together.
When aligned, the two programs improve patient care quality, efficiency, performance, and satisfaction. Also, by working closely to manage patients admitted by the ED, hospitals see improvements in metrics that improve patient care, including:
- EM left without treatment (LWOT) rates;
- EM door-to-provider times;
- ED length of stay (LOS) for admissions;
- Inpatient LOS.
When the two programs are at odds, however, their conflict has a ripple effect that increases cost, affects patient experience, patient safety, and physician satisfaction, and compromises care consistency.
For that reason, make it your priority to optimize EM-HM transitions of care by keeping lines of communication open and agreeing on process standards, mutual goals, accountability, and objective data measures.
Value Driver #2: Ensure an Accurate Case Mix Index
By capturing the severity of a patient’s illness — documenting the complications and comorbidities that accompany a diagnosis — you ensure that you assign the correct Diagnosis-Related Grouping (DRG) to a patient, ultimately prompting a more accurate (and improved) case mix index (CMI).
There are at least three reasons why this is important:
- The CMI is a reflection of the value of bundled DRG payments and advises the expected LOS;
- The CMI also impacts the quality scoring of patient outcomes by capturing the complexity of the case and ensuring more accurate reimbursement rates;
- Your ability to deliver appropriate documentation guidelines and collaborate with clinical documentation specialists can significantly improve the accuracy of the CMI for medical and surgical patients
Value Driver #3: Provide Efficient Rounding Practices, Resource Utilization
You can reduce the cost per case through efficient rounding practices and resource utilization. This includes appropriately focused lab tests and consultations, writing only clinically appropriate orders, and using medications listed on the hospital’s formularies when possible.
Value Driver #4: Maximize Value-based Performance Improvement
Medicare payment for services rendered is dependent on improved clinical quality through attention to CMS’s value-based programs. Effectively managing your HM program enables you to maximize performance on measures that reflect quality metrics.
Your goal should be to document improved efficiency, outcomes, and patient experience, while minimizing hospital-acquired conditions, mortality, and readmissions.
Value Driver #5: Reduce Avoidable Hospital Days (LOS)
The best way hospitals can improve their bottom line is by making beds available to admit additional patients. Patients who spend avoidable days in the hospital awaiting discharge require staffing and pharmaceutical resources while being exposed to preventable harm.
It is essential, then, that you manage patients well and discharge them as soon as there is no longer a clinical need for that bed.
Value Driver #6: Begin Discharge Planning, Post-discharge Management at Admission
Improving LOS not only requires the efficient ordering of tests, strategic use of consultants and specialists, and effective patient management but also the foresight to anticipate a patient’s discharge needs upon admission.
By assessing the patient’s probable discharge needs upon admission and working with case management, physical and occupational therapy, and nutrition, you can begin preparations to send the patient safely home with appropriate services or to a post-acute care setting at the outset.
Conclusion
By utilizing these six value drivers, your HM program can improve patient care and impact hospital profitability in ways you may never have imagined. By focusing on the quality and outcomes the value drivers promote, you offer a clear ROI for your hospital while also creating loyalty and satisfaction for patients and physicians alike.
To learn more about ways to increase HM program ROI, download the whitepaper “Maximizing Hospital Medicine ROI: Strategies to Optimize Your HM Program.”