The decision to employ providers does not lead to productivity or success on its own, but making small changes in the way you manage those providers can spur meaningful, sustainable shifts in your system and favorably impact your community.
In this white paper, we will discuss primary concerns and benefits for health systems with employed provider models, with key takeaways for hospital leaders such as:
- How to define the ideal profile of employed physicians in your facility or system
- What opportunities and issues accompany the hospital-employed provider model— and how to understand and address them
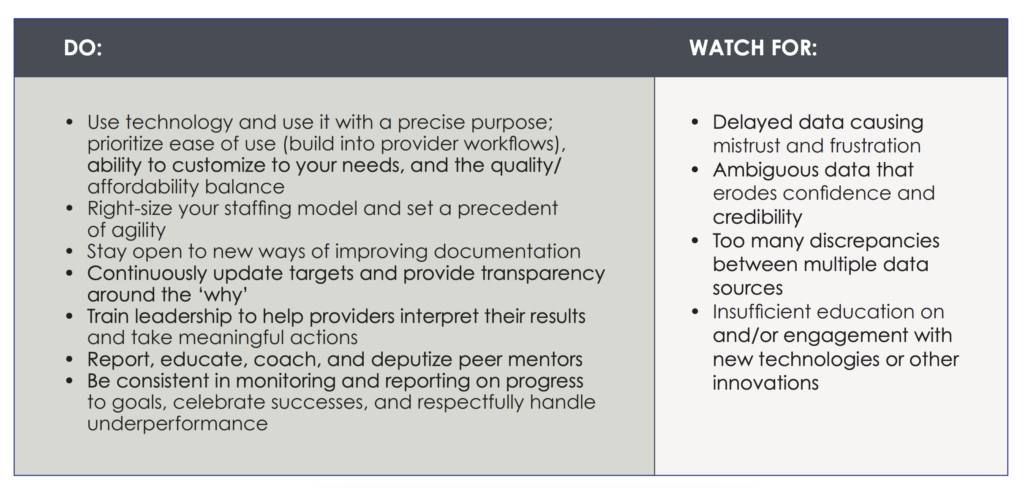
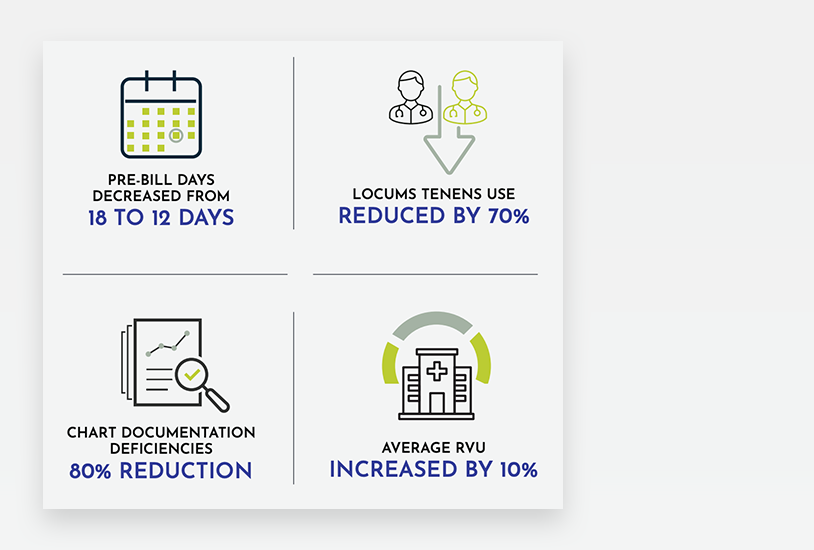
- How to manage in a way that positively impacts performance and productivity
- Ways to attain desired performance through critical success factors


 Introduction
Introduction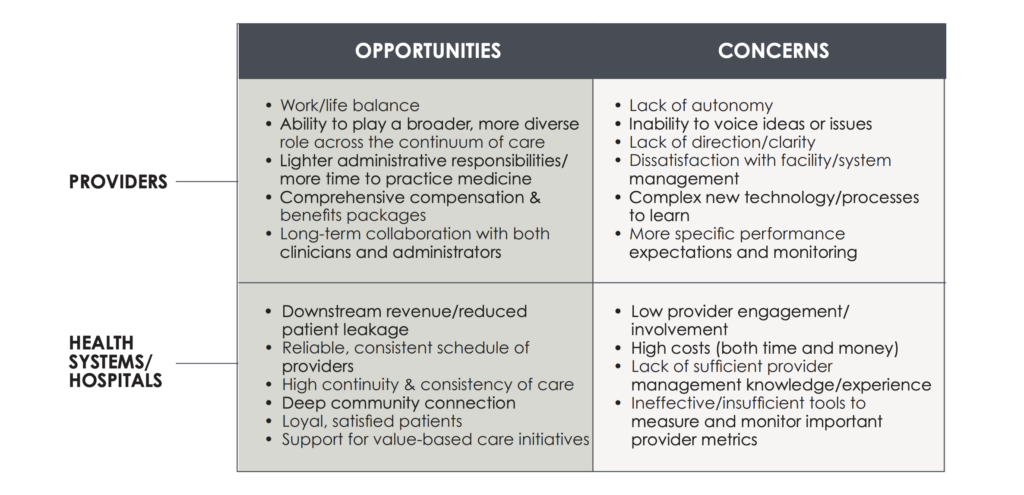
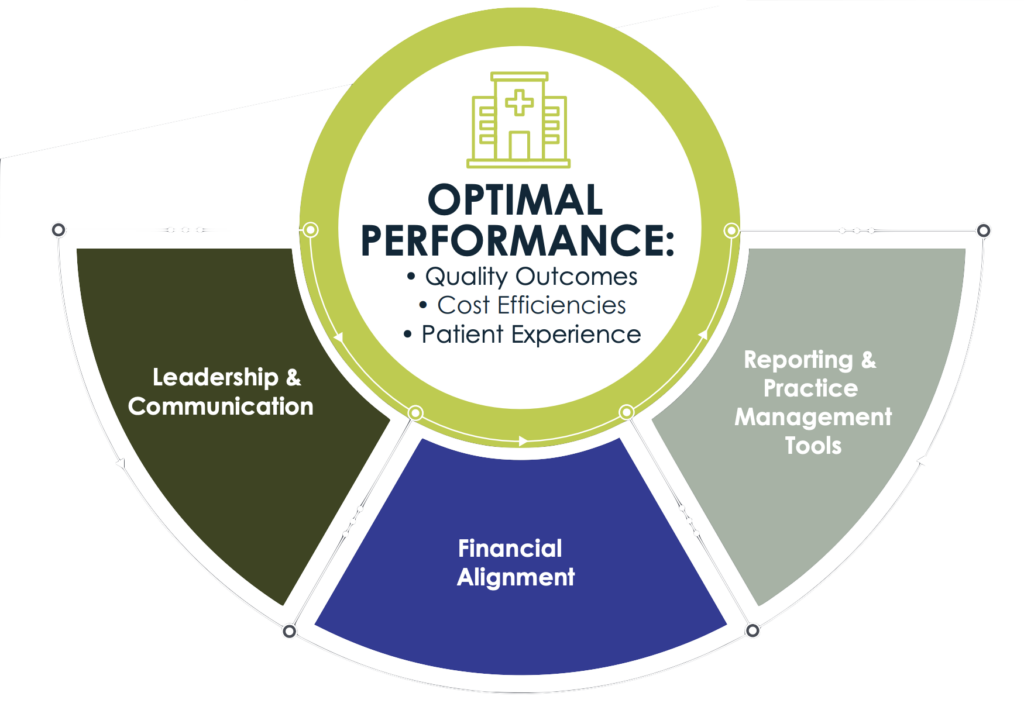
 Leadership & Communication
Leadership & Communication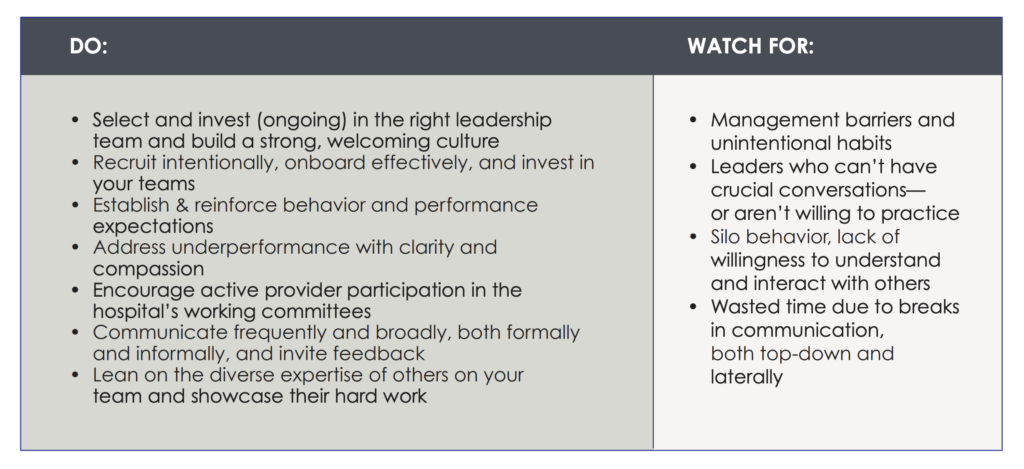
 Financial Alignment
Financial Alignment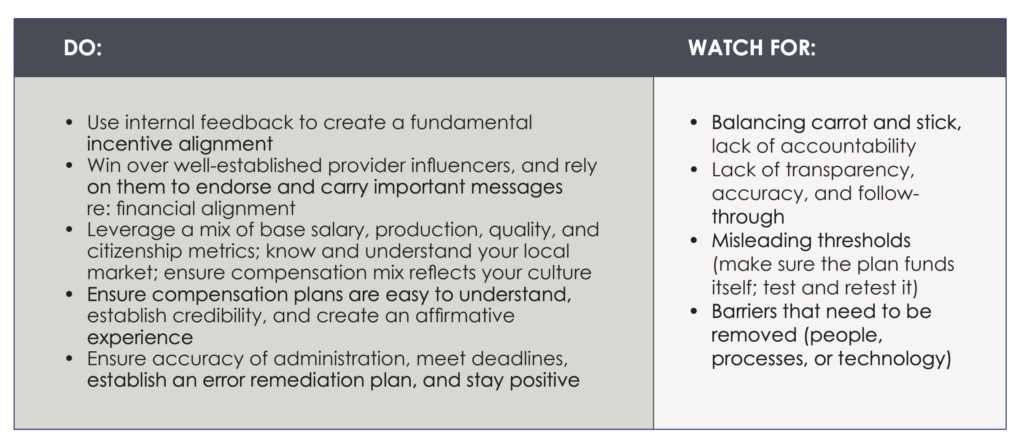
 Reporting and Practice Management Tools
Reporting and Practice Management Tools